The Healthcare sector has grown tremendously during these days and it left people with no choice during COVID times. Mostly, people are using the technology and several applications on this pandemic. These concepts of telehealth and telemedicine are very old, though it grabs full attention during the pandemic time. To make healthcare more efficient healthcare providers are seeking into the EHR and EMR.
What is EHR?
The readers may know the basic concept of EHR. It is a well-developed and very useful software that basically collects the data and stores it for future uses, it also integrates the data for the better multiple uses of it. It is the two-way interface software that is open for exchanging and sharing information anytime between the labs and pharmacy.
Healthcare with EMR:
EMR focuses on keeping the patient’s records, it stores the data and all the reports of patients on the server. It contains the medication data: the medicines and drugs given to the patient. The system is used in many clinics and small hospitals, but after using it, people are facing the one thing: the data with EMR can not be shared with anyone.
What is the difference between EHR & EMR?
The main difference between them is already mentioned while explaining both the systems. EMR is something that can not share the data outside the domain such as a clinic/ small hospital. Whereas EHR is the multi-sharing server that comprises and shares the data outside the core ie: to the labs and pharmacies.
One letter can really be a game-changer! EMR is considered to focus more on the patient’s reports and medical data. Whereas EHR it includes the demographics, results, medical history and medication history, and current illness.
What changes did the healthcare industry feel after using EHR & EMR?
From the surveys and reports, the doctors and healthcare providers have stated that the relationships are addressed very fairly after the use of EHR AND EMR has increased in healthcare. The professionals are finding it easy to correlate the patient’s data very fast.
EMR formats are fetching the data for the patients which are not so easily accessible for the doctors. Electronic care has the potential to achieve remarkable change in this field.
How does it make changes in providing care?
Traditionally, if we remember the system of the hospital at that time doctor’s used to write down all the details of the person manually, the doctor after running the hospital for long 10 years may have choked up with the data; the filing process and other detailing is the tough task.
But with the help of emerging technology; EHR provides us with the facility of maintaining data properly, the management of the files and also provides the assessment of the data.
Better workflows make better decisions:
The best thing about the EHR & EMR is that you can modify your workflows according to the person’s needs. Doctors and other professionals can make better decisions on how to work with that very efficiently.
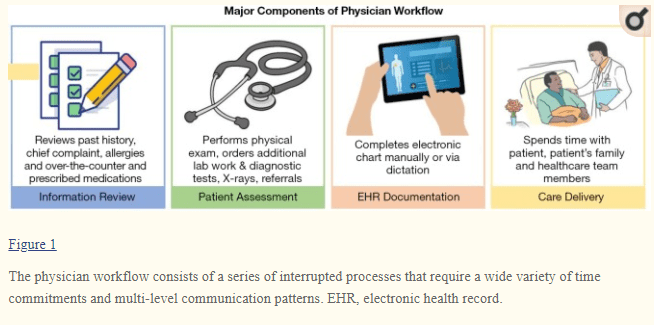
As figure 1 shows the major components of the workflow of the physician, it undergoes changes as information review> Patient assessment>> EHR documentation>>Care delivery.
If you compare the workflow of doctors in the early times then, the workflow was like, the first doctor walks into the labs to collect the reports, then he walks in for the X-Rays, and to the medical store also for checking the medicines prescribed earlier. Think about that situation where you wore the shoes of the doctor. By doing these for years the functionality and efficiency go decreasing.
There was no functionality in the doctor’s work till the EHR AND EMR got introduced to the world. But after the system got introduced to healthcare it makes it so easy for the professionals to check more patients with a good mind.
I am mentioning the word a good mind because; even the doctors sometimes get frustrated in roaming here and there for the stuff and he will not be able to provide the actual advice but after the system takes all the load; doctors will efficiently check more patients with the calmness in their behavior.
Key benefits of EHR:
- Sharing the files and information to different domains
- It is very precise and reliable for the patient
- Healthcare is very busy and hectic all the time, so using it is more convincing.
- It helps in maintaining the work-life balance
- The efficiency of the work will help to reach the goal faster.
Well, these are the general benefits of both sides, otherwise, it will suffice differently on both ends. Reading the benefits may not reflect much difficulty to you but as we all know small changes make the bigger things happen. Having the records and maintaining them is the biggest issue if this technology may not be invented.
If we compare the case of using papers and electronic health records, then there are many points that will clear you more.
Firstly, the implementation cost is higher compared to using papers and files, here you need to spend more and then it will be more functional for a longer period than the papers. The second thing is the use of manual strength is more in papers and in the case of EHR the manual strength using is very less.
As in using the paper and files, the need for furniture arises in storing the officials and a person to sequence them properly then too after the years the paper will turn yellow or the ink will smudge up. In order to find all the data secure after longer times, electronic data is saved in the cloud and the cloud data is secured very well.
Sometimes there is a risk of the documents being stolen, or being worried about the page quality. Or sometimes there’s a fear of misusing the documents. Whether in the case of electronic health records all these fears get changed into assurance. The data is secured by security features; the person with password access can access the data.
EHR Interoperability for healthcare
Interoperability is defined by the term “two-way use “, it means that if there are systems that are working with more than two systems for the data exchange or we can call it as data management. Artificial intelligence has correlated with interoperability for better transparency and analytics in the data. There are many levels of interoperability as I mentioned all in the article. I am sure by reading the whole article on EHR interoperability you will gain the knowledge of it in one place only, you do not need to fetch the articles more on it.
Electronic health records are very useful to safeguard confidential data. Here readers have the question in their mind, what is interoperability? How does it actually work? You have read many articles about interoperability
What is interoperability?
Interoperable is the system that allows the electronic sharing of information between EHR systems and healthcare professionals. It will improve the interoperability or we can say that it can improve the ease of the information available to the patients and the doctors.
Sometimes the system service requirements will differ according to the size of the clinics and state needs. EHR systems choose specific systems in accordance to provide care and medications.
In general, if we see it is just the ability of systems for sending and receiving the different types of data exchange with the authentication and security. It will help to send the information to the individual desk very quickly.
EHR interoperability ecosystem:
The ecosystem of interoperability consists of an individual, system, and processes. It will be defined as per the needs of the patients. The healthcare providers are efficiently working as per their abilities and requirements.
Why is Interoperability is important in healthcare?
Interoperability is very important in healthcare because it deals with the information, whether it is the doctor’s perspective details or whether it is from the patient’s side. The confidential data needs to provide attention and specific care; well the electronic system provides it in a more efficient way.
There’s always a fear of paradox in maintaining the data and security; to secure the data management also proves to be very useful, in the smaller scale if you think of just one hospital then too the data sharing of just 24hrs would be more than anyone can think of.
Now just think at the larger scale, the populations in the developing countries are high, the diseases and the no. of patients are increasing day by day; think of the situation where all the hospitals and their data management has to be done by the professionals.
In addition to helping the physicians and the professionals, the system covers almost all the queries of the professionals; various interoperability organizations have developed across the country worldwide. Also, the medical decision-makers started keeping the records of the patients to do research and surveys and provide better techno solutions.
Government service providers are also interested in the upcoming use of interoperability in providing good service delivery in every sector. The government is demanding different models of interoperability to assist the care according to the requirements and needs of the different stakeholders.
What is FHIR?
The full form of FHIR is the fastest health interoperability resource, it organizes data with the medications, patient’s implications, and provides the different workflow data. In various countries like the USA, Canada has already accepted the FHIR, systems for better applications and will provide better care with solving the implications.
It seems that FHIR is the standard format, then the expectations from the vendors are increasing day by day. Many institutions want the modification in the information that also the system is providing many changes and new methods with healthcare records.
The health exchanges and interoperability:
With modern innovations, consumers have better demand for changes involving exchanges and interoperability.
Standardization format:
The standard format is needed for the data exchanges; vendors are providing EHRs with the modification with the APIs to develop the efficiency in the system. Many providers are using the customized format as per their needs and advancement.
Authentication:
The system is providing proper authentication and security in the medical field. The data is not accessible to all the members but is hardly accessed with the passwords, the system proves to be very secure and authenticated.
Assent:
In digital health systems, information is moving from provider to provider. The Healthcare industry is becoming more cautious in maintaining data management.
Professional burdens:
Professional tools are used in keeping the healthcare record data, it is helpful in keeping the standardized format and it helps in billing and execution for the medical job operation. Professionals’ burdens are natural in the behavior because the professionals are engaging with really massive data management.
There are some levels of interoperability mentioned below::
Foundational:
It deals with the system that only helps to receive the data from the system and is not prone to exchange or change the information.
Structural:
This is a more complex stage where the system is prone to exchange the data by allowing the syntax, but it is not able to interpret the data at the first level.
Semantic:
In this stage, the system is able to interpret, receive or exchange the data.
Organizational:
In this stage, organizational interoperability allows the non-technical to carry the things like designing the workflows, maintaining the tasks, and confining the changes.
What are the key benefits of interoperability?
- The first and foremost thing is the data exchange; the patient’s access to the data is secured and data management is the key concern to deal with it.
- It can be more helpful to labs, hospitals, pharmacy, in maintaining the workflows.
- It is helpful in triggering in managing the official workflows very quickly.
- EHR EMR integration is the new solution in the healthcare industry for better advancements.
Conclusion:
We have seen the benefits of EHR; also the concept and use of the technology with its proper use. The Healthcare sector is the field on which every single person is dependent. To make the care efficient it is more important to accept the new systems; make trial and error sessions and if it works efficiently and productively then the providers convey the use of that technology. The EHR EMR integration works best and provides the best result. The crux is that technology is demanding the good, for the good in the medical field, technological advancements help to exchange the data securely, minimization of the resources and security is the good feature. EHRs and EMRs are useful in maintaining the records from various platforms. The healthcare mobile app developers and professionals are really happy with the innovations.


